Cancer is one of the most feared diseases of modern times, affecting millions of people around the world. Despite the advances in medicine, early detection, and treatment, cancer remains a leading cause of death globally. To effectively fight this complex disease, it is essential to understand not only its biological mechanisms but also the patterns and trends in how it develops and spreads across populations. This is where cancer epidemiology comes into play. Cancer epidemiology is a scientific field dedicated to studying the distribution, causes, and risk factors of cancer in human populations. It provides insights that guide prevention, early detection, and public health strategies. Understanding this field is critical for both medical professionals and the general public, as it allows us to make informed decisions about health policies, lifestyle changes, and research priorities.
Understanding Cancer Epidemiology
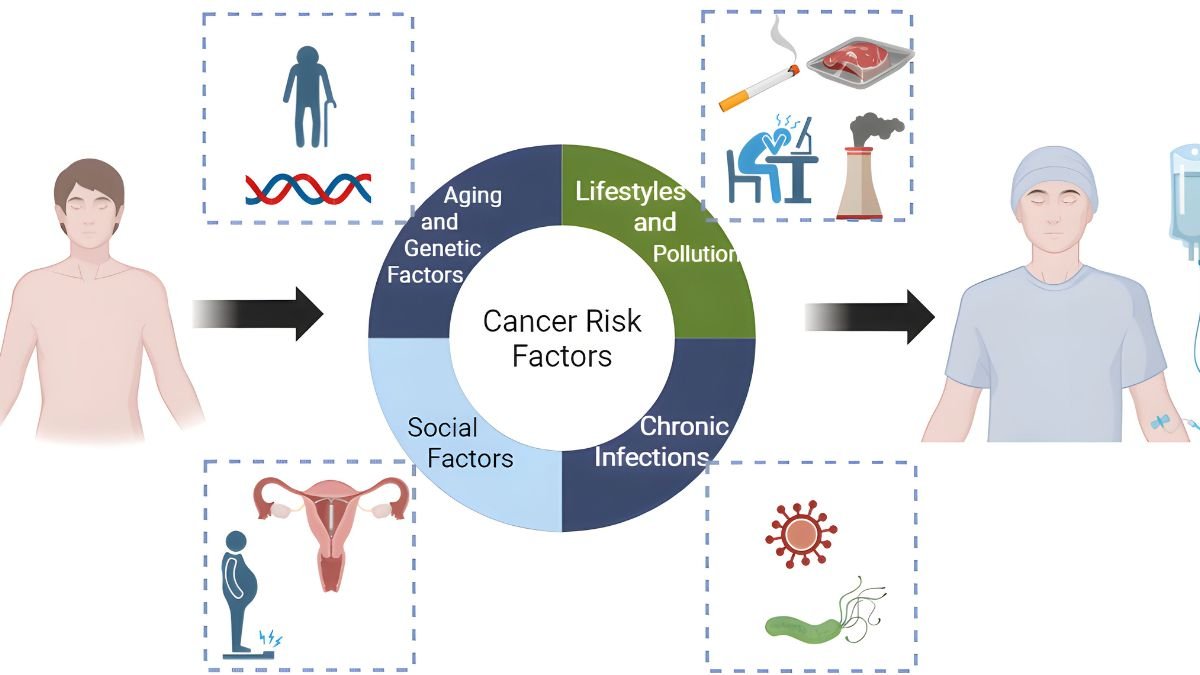
At its core, cancer epidemiology is the study of cancer in populations rather than in individual patients. While clinical research focuses on understanding how cancer affects a single person and how to treat it, epidemiology looks at larger trends to uncover patterns that might not be obvious on an individual level. Researchers in this field investigate questions such as: Which populations are most affected by certain types of cancer? How does age, gender, or ethnicity influence cancer risk? What environmental, genetic, or lifestyle factors contribute to the development of cancer?
By examining these questions, epidemiologists can identify both high-risk groups and potential preventive measures. For instance, studies have shown that certain cancers are more common in specific age groups or geographic regions. Lung cancer is notably prevalent among smokers, whereas skin cancer rates are higher in populations with prolonged sun exposure and lighter skin. These observations allow health authorities to develop targeted screening programs and awareness campaigns.
The Role of Cancer Epidemiology in Prevention
One of the most powerful aspects of cancer epidemiology is its role in prevention. Unlike some diseases that can only be treated once they appear, many cancers have identifiable risk factors that can be managed or avoided. By studying large populations, epidemiologists can uncover these risk factors and provide evidence-based recommendations to reduce cancer incidence.
For example, extensive epidemiological research has linked cigarette smoking with lung cancer. This evidence has formed the foundation of anti-smoking campaigns, tobacco regulations, and public health initiatives worldwide. Similarly, studies on diet, obesity, and physical activity have revealed connections to cancers such as colorectal, breast, and pancreatic cancer. These findings allow governments, organizations, and individuals to take proactive steps in reducing exposure to harmful behaviors and environmental factors.
Cancer epidemiology also plays a role in vaccination and early detection strategies. The link between human papillomavirus (HPV) and cervical cancer led to the development of the HPV vaccine, which has dramatically reduced the risk of cervical cancer in vaccinated populations. Similarly, understanding the risk factors for liver cancer has informed hepatitis B vaccination programs in many countries, showing how epidemiology directly influences preventive medicine.
Identifying High-Risk Populations
Cancer does not affect all populations equally. Epidemiological studies often reveal significant disparities in cancer incidence and outcomes based on demographic, geographic, and socioeconomic factors. Identifying high-risk populations is essential for designing effective interventions.
For instance, African American men have a higher incidence of prostate cancer compared to other ethnic groups, while certain genetic mutations, such as BRCA1 and BRCA2, dramatically increase the risk of breast and ovarian cancers in women. Geographic differences also exist; stomach cancer is more prevalent in East Asia, while melanoma rates are higher in countries with strong sun exposure like Australia. Understanding these patterns helps public health officials prioritize screening programs, allocate resources effectively, and educate communities about specific risks.
Socioeconomic factors also play a critical role in cancer risk and survival. People with limited access to healthcare or low-income communities often face delayed diagnoses, limited treatment options, and higher mortality rates. Epidemiology helps to uncover these inequalities, providing a basis for policy changes aimed at reducing disparities and ensuring that cancer prevention and treatment are accessible to all.
The Importance of Cancer Registries
Cancer epidemiology relies heavily on data collected through cancer registries. These registries track new cancer cases, monitor trends over time, and provide researchers with valuable information about cancer incidence and survival rates. Without accurate data, it would be impossible to understand the true burden of cancer or evaluate the effectiveness of interventions.
Cancer registries allow for comparisons between regions, countries, and even continents. They help identify emerging patterns, such as increases in certain cancers linked to lifestyle changes or environmental exposures. They also track long-term outcomes for cancer patients, which is essential for improving treatment strategies and healthcare planning.
For example, registries in high-income countries often show improvements in survival rates due to early detection and advanced treatments. Conversely, in low- and middle-income countries, data may highlight areas where resources are lacking and where targeted interventions are urgently needed. These insights are crucial for global health planning and for organizations that aim to reduce cancer-related deaths worldwide.
Research and Clinical Applications
Beyond prevention and public health, cancer epidemiology contributes directly to research and clinical practice. Epidemiologists often collaborate with medical researchers to identify potential causes of cancer, understand tumor biology, and evaluate new treatment approaches. Their work provides the foundation for clinical trials, ensuring that studies are designed based on patterns observed in large populations.
For example, understanding the epidemiology of colorectal cancer has led to the development of screening methods such as colonoscopy, which can detect precancerous growths before they become malignant. Similarly, research on breast cancer incidence has informed recommendations for mammography screenings, particularly for women over a certain age or those with a family history of the disease.
Epidemiological studies also guide public health campaigns and policy-making. Governments rely on evidence from population studies to implement smoking bans, dietary guidelines, vaccination programs, and occupational safety regulations. Without this data, efforts to reduce cancer incidence would be largely guesswork rather than informed strategy.
Global Impact of Cancer Epidemiology
Cancer is a global health issue, and epidemiology provides the tools needed to tackle it on an international scale. The World Health Organization and other global health agencies use epidemiological data to identify trends, allocate resources, and prioritize research efforts. By comparing cancer patterns across countries, researchers can better understand how lifestyle, environment, and healthcare systems influence cancer risk and outcomes.
Global epidemiological studies have highlighted the rise of certain cancers in low- and middle-income countries, often linked to changes in diet, urbanization, and increased life expectancy. This knowledge enables international collaborations aimed at prevention, early detection, and treatment improvements. In many ways, cancer epidemiology acts as a bridge between science and policy, connecting research findings with practical interventions that save lives.
Challenges in Cancer Epidemiology
While cancer epidemiology provides invaluable insights, it also faces several challenges. One major issue is the complexity of cancer itself. Cancer is not a single disease but a collection of related diseases with different causes, progression patterns, and responses to treatment. This diversity makes it difficult to pinpoint exact risk factors and design universal prevention strategies.
Data quality and accessibility also pose challenges. In many regions, especially in low-income countries, cancer cases may go unreported or be misclassified. Limited healthcare infrastructure can result in incomplete or delayed data, making it harder for epidemiologists to identify trends and high-risk populations accurately.
Moreover, the interactions between genetic, environmental, and lifestyle factors are incredibly complex. For instance, two people with the same exposure to a carcinogen may experience very different outcomes based on their genetic makeup, diet, or overall health. Epidemiologists must use sophisticated statistical methods to account for these variables, but uncertainty can never be fully eliminated.
The Future of Cancer Epidemiology
Despite these challenges, the future of cancer epidemiology is promising. Advances in technology, data analytics, and genomics are providing unprecedented opportunities to study cancer at both population and molecular levels. Large-scale biobanks, genetic databases, and digital health records allow researchers to identify patterns and risk factors more accurately than ever before.
Artificial intelligence and machine learning are also revolutionizing the field. These tools can analyze massive datasets to uncover hidden correlations, predict cancer risk, and optimize screening strategies. Personalized medicine, informed by epidemiological insights, is increasingly becoming a reality, allowing treatments and prevention strategies to be tailored to an individual’s genetic profile and lifestyle.
International collaboration will continue to be essential. By sharing data, resources, and expertise, countries can collectively combat cancer more effectively. Global initiatives aimed at reducing cancer incidence and improving survival rates rely heavily on the insights provided by cancer epidemiology.
Conclusion
Cancer epidemiology is a vital field that bridges the gap between science, medicine, and public health. By studying the distribution, causes, and risk factors of cancer in populations, epidemiologists provide the knowledge needed to prevent disease, identify high-risk groups, and develop effective interventions. Their work informs public health campaigns, shapes healthcare policy, and guides research efforts around the world.
Understanding cancer epidemiology is not just the responsibility of scientists or medical professionals—it is also essential for individuals and communities. Knowledge of risk factors, lifestyle influences, and preventive measures empowers people to make informed choices that can reduce their risk of cancer. As research continues and technology advances, cancer epidemiology will remain at the forefront of efforts to reduce the global burden of this complex disease, saving countless lives and improving public health worldwide.