Stress has become an inescapable part of modern life. Whether it’s the pressure of work, personal relationships, or financial struggles, the constant demands on our mental and emotional resources can leave lasting impacts on our health. While occasional stress can sometimes motivate us to act or perform better, chronic stress—persistent stress over a long period—can have far-reaching consequences. One of the most serious effects of chronic stress is its impact on long-term health, particularly for individuals who already suffer from chronic health conditions. Understanding the relationship between stress and chronic illness is crucial for managing both mental and physical well-being.
The Physiology of Stress
Stress triggers a complex physiological response in the body, commonly known as the “fight or flight” response. When a stressful situation arises, the brain signals the adrenal glands to release hormones such as cortisol and adrenaline. These hormones prepare the body to respond quickly by increasing heart rate, blood pressure, and blood sugar levels. In the short term, this response can be beneficial, allowing us to react to immediate threats efficiently.
However, when stress becomes chronic, the body remains in a heightened state of alert for extended periods. Constant exposure to stress hormones can lead to detrimental changes in the body, including inflammation, immune suppression, and hormonal imbalances. These changes make it harder for the body to maintain equilibrium, setting the stage for the development or worsening of chronic health conditions.
Stress and Cardiovascular Health
One of the most direct links between stress and chronic health conditions is its impact on the cardiovascular system. Chronic stress is known to increase blood pressure, elevate heart rate, and cause arterial inflammation, all of which contribute to the risk of heart disease. People under prolonged stress are also more likely to engage in unhealthy behaviors such as smoking, overeating, or neglecting exercise, which further exacerbate cardiovascular risk.
Research has shown that stress can contribute to the development of atherosclerosis, a condition in which arteries become narrowed and hardened due to plaque buildup. Over time, this can lead to heart attacks, strokes, or other serious cardiovascular events. For individuals with pre-existing conditions like hypertension or heart disease, stress can worsen symptoms and increase the likelihood of complications.
Stress and Diabetes
Chronic stress can also have a significant impact on metabolic health, particularly in people with diabetes. Stress hormones like cortisol raise blood glucose levels by signaling the liver to release stored sugar. While this mechanism is helpful in acute stress situations, persistent elevation of blood sugar can be dangerous for those with diabetes or prediabetes.
In addition to affecting glucose metabolism, stress may influence insulin sensitivity. People under chronic stress may find that their body’s ability to use insulin effectively decreases, leading to higher blood sugar levels and an increased risk of complications. Stress can also interfere with daily diabetes management routines, such as medication adherence, monitoring blood sugar, or maintaining a healthy diet, creating a vicious cycle of worsening health outcomes.
Stress and Autoimmune Disorders
Autoimmune disorders, in which the immune system mistakenly attacks healthy tissues, are particularly sensitive to the effects of stress. Conditions such as rheumatoid arthritis, lupus, and multiple sclerosis often flare up in response to psychological or emotional stress. This occurs because stress hormones can dysregulate immune function, triggering inflammation and exacerbating symptoms.
For example, individuals with rheumatoid arthritis may experience increased joint pain and stiffness during periods of high stress, while those with lupus may notice more frequent or severe flare-ups. Stress management strategies, therefore, are often recommended as part of the treatment plan for autoimmune disorders, alongside medications and lifestyle interventions.
Stress and Gastrointestinal Health
The gut is often referred to as the “second brain” due to the complex network of nerves and neurotransmitters that regulate digestive function. Stress can significantly affect gastrointestinal health, leading to symptoms such as stomach pain, bloating, diarrhea, or constipation. Chronic stress can also exacerbate conditions like irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), and inflammatory bowel disease (IBD).
When stressed, the body redirects blood flow away from the digestive system to prioritize muscles and the brain for immediate action. This can disrupt digestion, nutrient absorption, and gut motility. Over time, chronic stress may contribute to inflammation in the gut, altering the balance of beneficial bacteria and worsening gastrointestinal conditions.
Stress and Mental Health
While stress has obvious physical consequences, its impact on mental health is equally important. Chronic stress is closely linked to anxiety, depression, and other mood disorders. Mental health challenges, in turn, can worsen physical health outcomes, creating a feedback loop that is difficult to break.
For individuals with chronic health conditions, stress can amplify feelings of helplessness or fatigue, reduce motivation to adhere to treatment plans, and decrease overall quality of life. The emotional burden of managing a long-term illness combined with stress can lead to what is sometimes called “psychological comorbidity,” where mental health issues and chronic disease interact and compound one another.
Behavioral Consequences of Stress
Beyond physiological changes, stress often drives behaviors that negatively impact health. People under stress may turn to unhealthy coping mechanisms, such as smoking, alcohol consumption, overeating, or avoiding exercise. These behaviors not only worsen chronic health conditions but also create additional challenges in managing stress itself.
For instance, someone with hypertension may rely on high-sodium comfort foods when stressed, leading to further blood pressure increases. Similarly, stress-induced sleep disturbances can reduce the body’s ability to repair itself, increase inflammation, and weaken immunity. Understanding these behavioral consequences is key to breaking the cycle of stress and chronic illness.
Strategies to Manage Stress and Protect Health
Managing stress is not just about improving mental well-being—it is a crucial component of preventing and controlling chronic health conditions. Effective strategies can include mindfulness practices, physical activity, social support, and professional counseling.
Mindfulness techniques such as meditation, deep breathing, and yoga have been shown to reduce stress hormone levels, lower blood pressure, and improve mood. Regular physical activity helps regulate stress by releasing endorphins, improving circulation, and promoting better sleep. Social support, whether from friends, family, or support groups, provides emotional resilience and a sense of connection that can buffer against stress.
Professional counseling or therapy can also help individuals develop healthy coping mechanisms, address underlying mental health issues, and navigate the challenges of living with chronic illness. Incorporating stress management into a broader treatment plan is often essential for long-term health improvement.
Conclusion
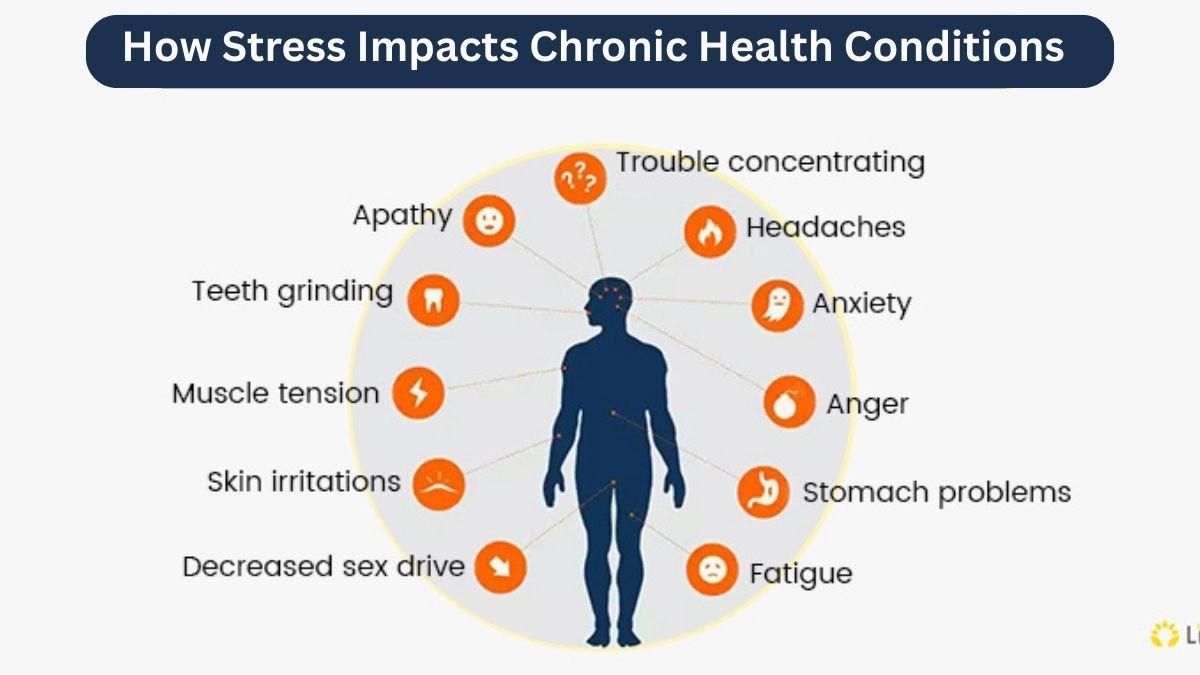
Stress is an inevitable part of life, but its effects on chronic health conditions can be profound and far-reaching. From cardiovascular disease and diabetes to autoimmune disorders and gastrointestinal problems, chronic stress alters the body’s physiological balance, triggers inflammation, and worsens symptoms. Additionally, stress can influence mental health and drive behaviors that further compromise well-being.
Understanding the connection between stress and chronic health conditions highlights the importance of proactive management. Incorporating stress-reduction strategies, cultivating resilience, and seeking support when needed can significantly improve quality of life and health outcomes. By addressing stress not as a minor inconvenience but as a serious factor in chronic illness, individuals can take meaningful steps toward better physical and mental health.